Research Groups
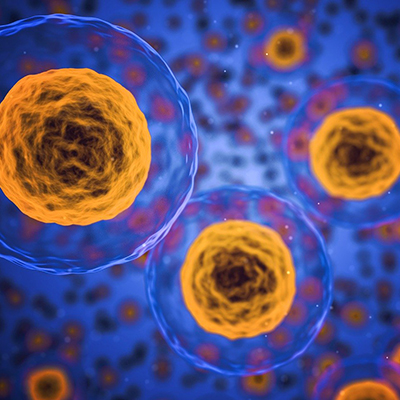
We are changing the future of health and well being
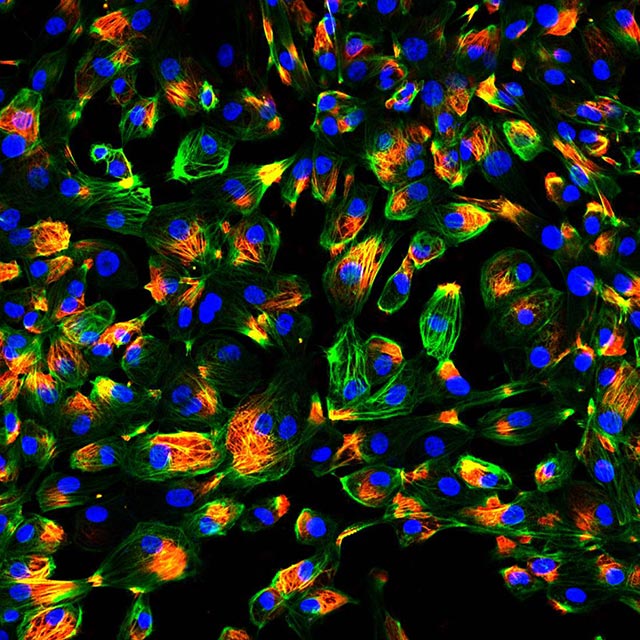
Our research marks the beginning of a new future. Exploring the molecular realm, we examine the smallest units of life to discover how the world works. We continually push the boundaries of the scientific frontier, searching for answers to some of the world’s most challenging problems.
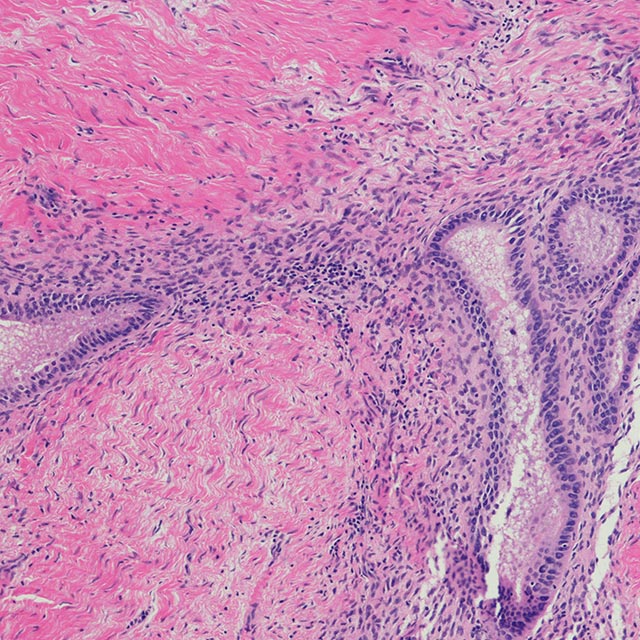
Centre for Cell Biology of Chronic Disease Centre for Chemistry and Drug Discovery Centre for Superbug Solutions Centre for Population and Disease Genomics
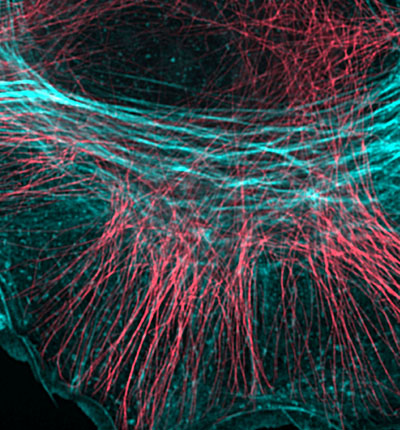
Critical Care Research Group
Professor John FraserPhysiology of circadian rhythms
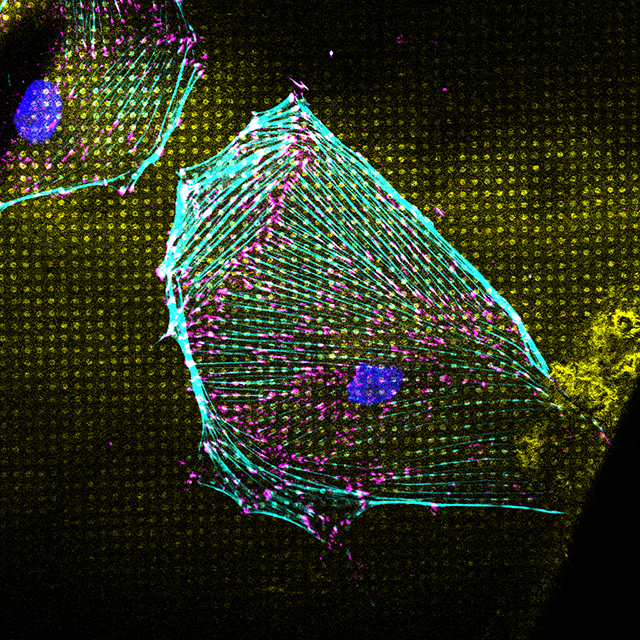
Associate Professor Frederic GachonCadherin cell-cell adhesion
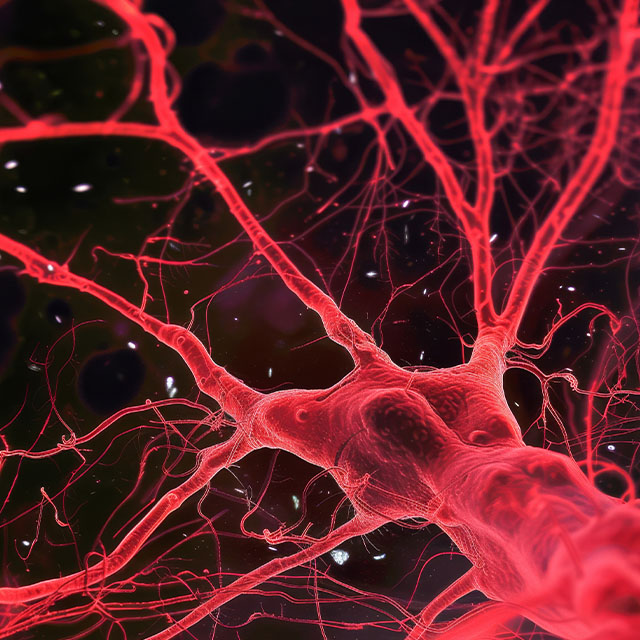
Professor Alpha YapCellular mechanisms to maintain a healthy vasculature
Dr Anne LagendijkCellular reprogramming and ageing
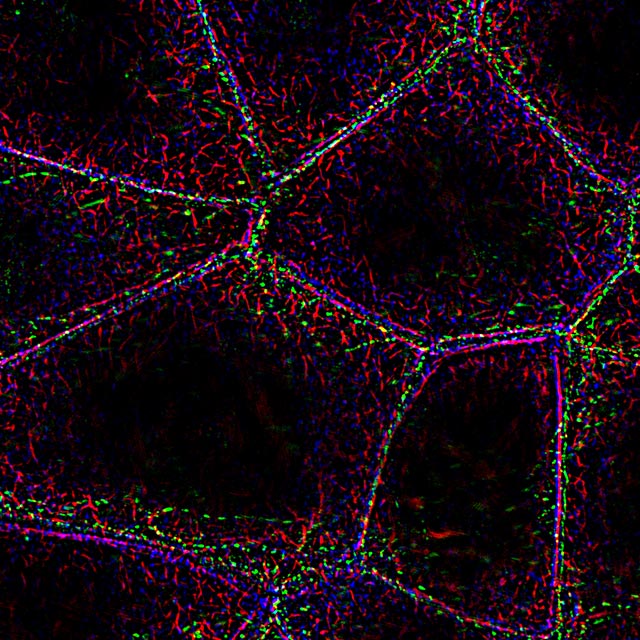
Dr Christian NefzgerStem cells and cardiovascular development
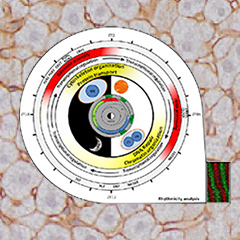
A/Prof Nathan PalpantMultiscale analysis of cellular membrane function
Professor Rob PartonInflammasomes
Professor Kate SchroderProtein trafficking and inflammation
Professor Jennifer StowInnate immunity, infection and inflammation
Professor Matt SweetDynamics of morphogenesis
Dr Mel WhiteMolecular Mechanisms of Neurological Disease
Professor Michael O'Sullivan
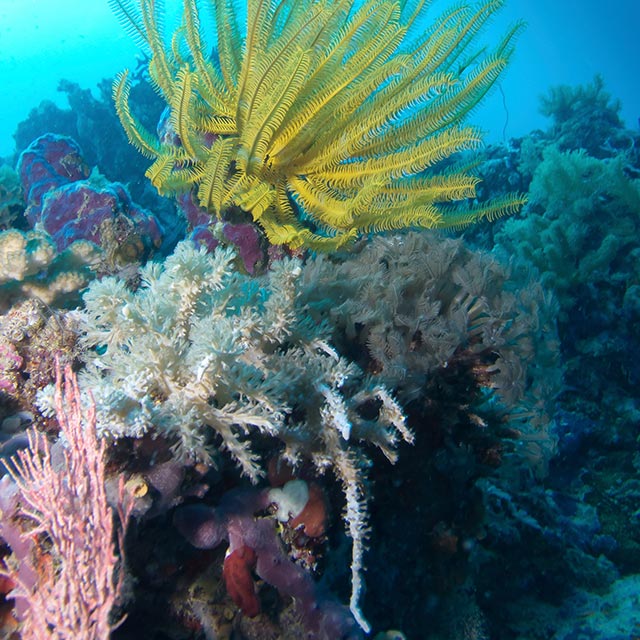
Molecular biodiscovery: learning from nature
Professor Rob CaponProtein structure in drug and insecticide design
Professor David CraikChemistry and human therapeutics
Professor David FairlieBioinspired design of solar biotechnology systems
Professor Ben HankamerBugs and drugs
Professor Glenn KingPharmacology of marine toxins
Professor Richard LewisNeuropeptide research
Associate Professor Markus MuttenthalerCombinatorial chemistry and molecular design
Associate Professor Mark Smythe
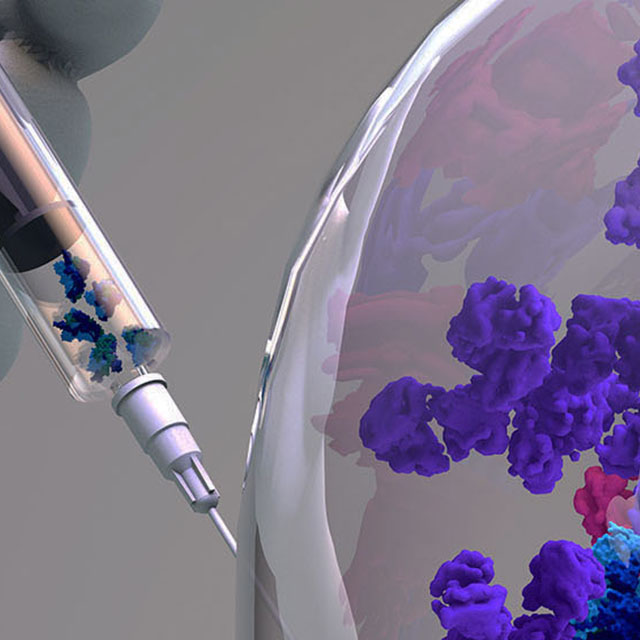
Discovering new ways to make better cancer drugs
Dr Conan WangMolecular mechanisms of blood-brain barrier transport
Dr Rosemary Cater
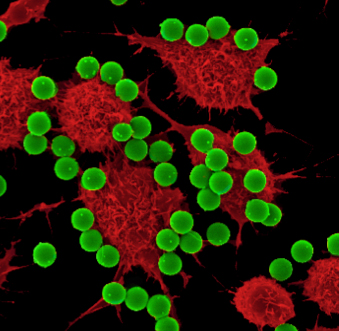
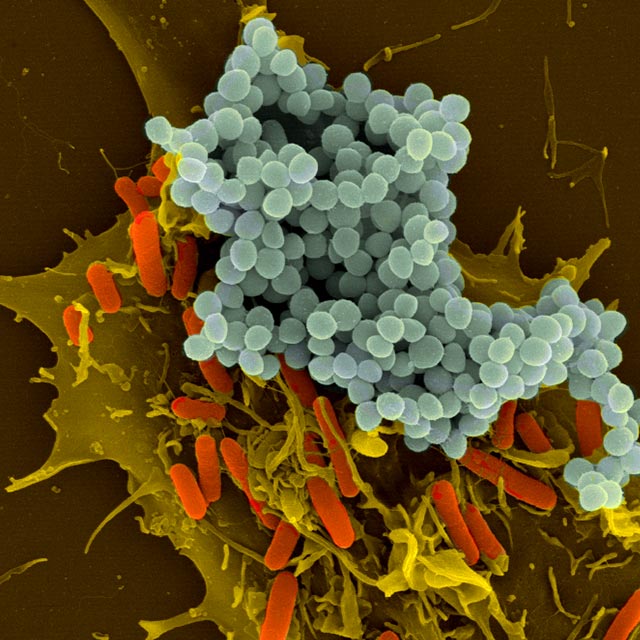
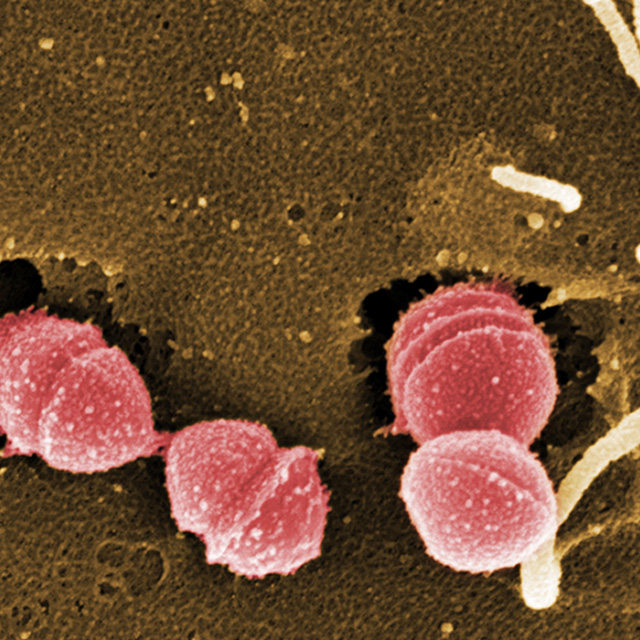
Superdrugs vs Superbugs
Professor Mark BlaskovichImmunology of infectious disease
Professor Denise DoolanBacterial infections and immunology
Professor Ian Henderson
Bacterial pathogenesis and antibiotic resistance
Professor Mark SchembriBacterial cell wall
Professor Waldemar VollmerStrep A pathogenesis and treatment
Professor Mark Walker
Microbial Genomics and Bioinformatics
Dr Brian Forde
Genetic Epidemiology
Professor David EvansSystems Genomics
Associate Professor Allan McRaeGenomics of reproductive disorders
Professor Grant MontgomeryGenomics and Machine Learning
Dr Quan NguyenProgram in complex trait genomics
Professor Peter Visscher, Professor Naomi WrayStatistical Genomics
Associate Professor Loic Yengo
Genomics in Health
Dr Sonia Shah
Research excellence
$1.3 billion+ commercial investment attracted to IMB research
1454 international collaborators
300+ original publications in 2022
$28M in research funding last calendar year
20%+ of patent families at UQ are derived from IMB research
100% of donations go to the cause
General enquiries
+61 7 3346 2222
imb@imb.uq.edu.au
Media enquiries
IMB fully supports UQ's Reconciliation Action Plan and is implementing actions within our institute.
Support us
Donate to research
100% of donations go to the cause