Matthew Cooper, The University of Queensland and Andrew Piggott, The University of Queensland
This article was originally published on The Conversation in 2011.
The rapid emergence of multidrug-resistant bacteria, or “superbugs” is a critical global health issue. Paradoxically, while there is a compelling need for new antibiotics, their development has slowed dramatically in recent years.
Between 1970 and 2000, the majority of approved antibiotics were based on one of five existing antibiotics.
While each new incarnation of an old drug is able to provide a few more years of antibiotic protection, they all inevitably succumb to the relentless pressures of bacterial resistance.
This is largely because they are all similar in structure to the original antibiotic on which they are based.
Something old, something new
In the “golden era” of antibiotic drug discovery – 1950 to 1970 – drug companies could afford to be choosy, selecting only the very best candidates for approval.
As a result, many potent antibiotics did not make the cut for development and were abandoned.
In recent years, there has been a growing appreciation of this untapped resource: a legacy of the time when pharmaceutical companies were still actively investing in antibiotic research.
Given the current crisis in antibiotic discovery, the time is right to revisit many of these potentially invaluable molecules in search of antibiotic scaffolds with novel modes of action.
Notably, the three most recently approved new antibiotics – linezolid (2000), daptomycin (2003) and retapamulin (2007) – actually belong to chemical classes first reported in 1978, 1987 and 1952, respectively.
These are prime examples of old antibiotics reborn as highly successful new therapeutics.
Linezolid is a member of a class of chemicals discovered by DuPont in 1970. They kill bacteria by blocking the production of proteins.
However, early clinical trials revealed the antibiotic produced liver toxicity, and their development was discontinued.
Twenty years later, Pharmacia & Upjohn (now part of Pfizer) generated a new version of the antibiotic that was no longer toxic, and that was very effective in treating resistant skin infections and pneumonia, including the superbugs vancomycin-resistant enterococci (VRE), and methicillin-resistant Staphylococcus aureus (MRSA).
It is currently the market leader for the treatment of MRSA, with sales in excess of $1.1 billion in 2010.
Daptomycin is an antibiotic isolated from a soil bacterium in the early 1980s by Eli Lilly.
Preliminary studies showed the compound to be highly effective in treating infections, and it too had a novel way of killing bacteria by blocking protein synthesis.
However, due to the presence of mild but reversible side, effects, it was also shelved. In 1997, Cubist Pharmaceuticals looked more carefully at these side effects.
By using of a new form of giving the antibiotic (called a dosing regimen), it was able to get a safe drug approval by the United States Food and Drug Administration in 2003.
This previously “forgotten” antibiotic has sales expected to top US$1 billion this year.
Retapamulin was first isolated in 1952 by members of the New York Botanical Garden.
Again, this antibiotic had a new way of killing bacteria, but it was not suitable to be taken orally (in tablet form) and was shelved.
Some 25 years later, GlaxoSmithKline resurrected retapamulin, recognising that while it could not be given orally, it could be given topically (as an ointment on the skin) for infections such as impetigo.
It is now marketed under the name “altabax” and is the first new topical antibiotic to be approved in almost 20 years.
Vancomycin was discovered in bacteria from the jungles of Borneo by a missionary, who in 1953 provided the sample to the drug company Eli Lilly.
It was used as the antibiotic of last resort, but in the 1990s resistant bacteria began to appear.
At the University of Queensland, we have made a new drug candidate based on vancomycin that is a thousand times more potent than the old antibiotic, and that can also kill resistant superbugs.
The future of antibiotics
As existing and new superbugs continue to spread unchecked throughout the world, radical and disruptive approaches to drug discovery and development are urgently required.
The examples above demonstrate that by going “back to the future” we can develop new antibiotics to combat super bugs.
This approach can also be financially rewarding for those companies brave enough to take this path less trodden.
It is possible, indeed probable, that the next blockbuster antibiotic is lurking in the dark recesses of historical literature and old company reports, waiting to be given new life through simple chemical modification or reformulation.
Even so, the cost of bringing an antibiotic to market is astronomically high at between $500 million and $900 million.
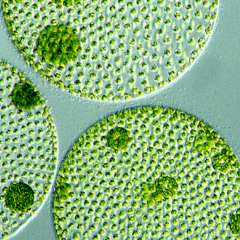
![]() To take advantage of the drugs we already have, we also need to encourage governments to help prime research in academia, and biotech and drug companies to address the perfect storm caused by a resurgence of superbugs and an empty pipeline of new antibiotics.
To take advantage of the drugs we already have, we also need to encourage governments to help prime research in academia, and biotech and drug companies to address the perfect storm caused by a resurgence of superbugs and an empty pipeline of new antibiotics.
Matthew Cooper, Prof. Institute for Molecular Bioscience, The University of Queensland and Andrew Piggott, Senior Research Officer in the Institute for Molecular Bioscience, The University of Queensland
This article was originally published on The Conversation. Read the original article.