A gene that helps to control inflammation increases the risk of obesity and could be turned off in mice to stop weight gain, a study co-led by Dr Denuja Karunakaran from the Institute for Molecular Bioscience at The University of Queensland found.
Dr Karunakaran said she was determined to unravel the links between inflammation and obesity that went deeper than excessive eating or lack of exercise.
“We found small changes in the inflammatory gene RIPK1 in the obese people, and these variations caused an increased amount of the gene being present in their fat tissue, increasing their risk of being obese,” Dr Karunakaran said.
“RIPK1 is essential for a healthy immune response, but it also causes hyper-inflammation when it ‘goes rogue’.
“By finding an increased amount of this inflammation-related gene in obese people, we can confidently say that inflammation increases the risk of obesity.”
The researchers then looked at the effect of turning the inflammatory gene on and off in mice.
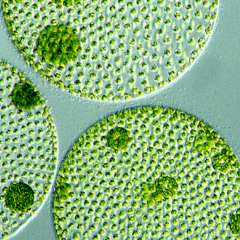
Fat tissue sparks immune response
Without the gene, the mice remained at a normal weight despite eating a high-fat diet and their risk of diabetes was reduced.
The mice with a normal level of the inflammatory gene put on weight from eating the same high-fat diet.
More than half the 2000 participants were extremely obese with an average Body Max Index of 41 and half were a healthy weight.
Dr Karunakaran said that when stores exceeded healthy levels, the fat tissue became overwhelmed, cells died and the immune system was activated.
“In obesity, the immune cells are working in overdrive, causing damaging inflammation when they don’t switch off,” she said.
“By understanding more about these inflammation pathways, we can find ways to intervene to treat obesity, especially in specific groups of people.
“These variations in the RIPK1 gene only occur in 8 to 12 per cent of the population – so maybe these are the people who struggle to lose weight despite doing all the right things.”
The study was co-led with Associate Professor Katey Rayner and conducted at The University of Ottawa Heart Institute.
This research was published in Nature Metabolism.
It was mainly funded by Canadian Institute for Health Research (CIHR), National Institute of Health, National Psoriasis Foundation and The University of Ottawa Heart Institute.